Bone health and Osteoporosis
Bone Structure
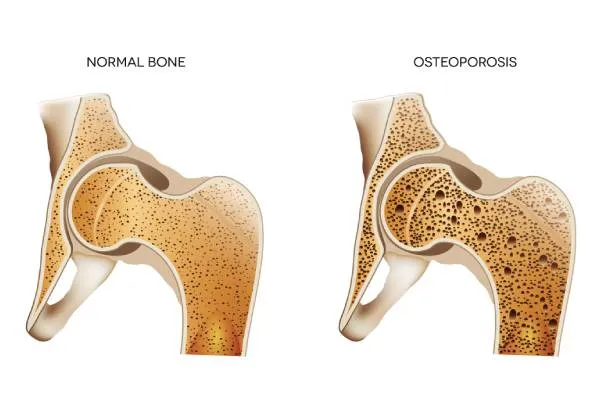
Bones are living tissue. There is dense outer layer of compact cortical bone (slow turn over) and central region made up of trabecular bone (rapid turnover). Trabecular bone is more susceptible to the effects of osteoporosis. Most osteoporotic fractures occur where there are high levels of trabecular bone e.g. vertebrae, hip and the wrist.
There are different types of bone cells; Osteoclasts which break down bone (resorption of the bone) and Osteoblasts which create new bone (formation of the bone).
Bone is constantly re-modelled and repaired due to damage caused by daily use. Remodelling is a balance process and there is equal amount of bone formation and bone resorption. In osteoporosis the net rate of bone resorption exceed rate of bone formation, these result in loss of bone mass, fragility and consequently bone fracture.
Osteoporosis
Osteoporosis is a progressive systemic skeletal disease characterised by low bone mass and strength of bone with a consequent increase in bone fragility and susceptibility to fracture. Its name comes from Latin for “porous bones.”
Osteoporotic fractures affect 1 in 3 women and 1 in 5 men over the age of 50. Osteoporosis leads to nearly 9 million fractures annually worldwide.
Osteoporosis can be present for years without any symptoms, but may cause severe back pain, loss of height over time, stooped/humped posture and bone fractures from minor injury.
Risk factors for Osteoporosis
- Age- bone mineral density (BMD) decreases with age
- Hormones- lower levels of oestrogen after menopause accelerate bone loss
- Premature menopause or hysterectomy (removal of the womb)
- Gender- women are at increased risk of osteoporosis as they start out with smaller bones and bone mass compared to men
- Family history of osteoporotic fracture
- Long term steroid use
- Treatment for breast cancer
- Endocrine problems: Hyperparathyroidism, Hyperthyroidism, Diabetes
- Other medical conditions: Coeliac disease, malabsorption syndromes, inflammatory bowel disease, eating disorders, Kidney diseases, Rheumatoid arthritis and Lupus
- Medicines used for the treatment of stomach ulcer and acid reflux, epilepsy medicines
- Low calcium and vitamin D
- Smoking
- Alcohol
- Low body Weight
Diagnosis of Osteoporosis
All postmenopausal women aged ≥50 years and patient with any of the above risk factors should be assessed for osteoporosis risk. Osteoporosis can be detected on special bone scans such as Dual Energy X-ray Absorptiometry (DEXA) or quantitative CT scan (QCT Bone Mineral Densitometry). Blood tests are performed to rule out other causes of osteoporosis.


Treatment of Osteoporosis
Some of the most important aspects of preventing osteoporosis include eating a healthy diet, doing regular exercise, avoiding smoking and taking Calcium and vitamin D supplements in recommended doses. If you have already been diagnosed with osteoporosis, medicines are available that can slow further loss of bone or increase bone density. These specific drugs include Bisphosphonates, Denosumab and Teriparatide.
With a wide range of osteoporosis medications available, it’s understandable to wonder which one is best for you. The decision about which treatment is right for you, and how long you need to take it, depends on your personal circumstances. At Healthbay, department of Rheumatology, you can discuss the best available treatment option for Osteoporosis with a qualified Rheumatologist.
About the author
Dr Mohammad Tariq (MBBS, MRCP UK, MRCP Rheumatology, FRCP Glasg) is a UK certified Rheumatologist who specializes in the management of arthritis and auto-immune diseases and metabolic bone diseases (Osteoporosis). He has broad knowledge and clinical experience in the management of metabolic bone diseases/Osteoporosis and newer therapies. Dr Tariq is a member of British Society of Rheumatology and Fellow of Royal College of Physicians UK.
Book a comprehensive checkup package for joint (arthritis) and bone health, call 800 4272 or email [email protected]